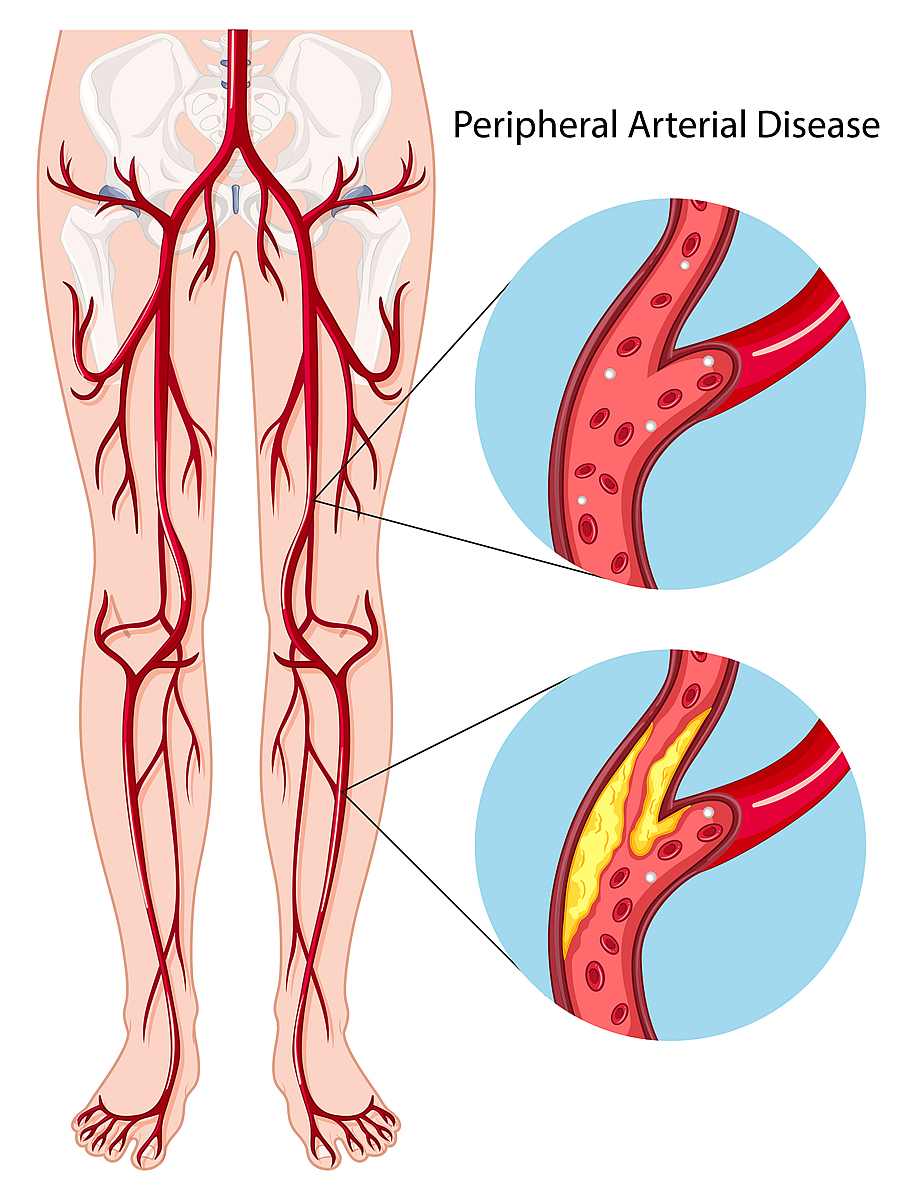
Peripheral Arterial Disease (PAD or PVD)
Peripheral artery disease (also called peripheral arterial disease) is a common circulatory problem in which narrowed arteries reduce blood flow to your limbs.
When you develop peripheral artery disease (PAD), your extremities — usually your legs — don’t receive enough blood flow to keep up with demand. This causes symptoms, most notably leg pain when walking (claudication).
PAD is relatively common, affecting more than 10 million people in the U.S. It is more common in people who are 65 or older, but can occur at nearly any age. Smoking; high blood pressure; high cholesterol or triglycerides; diabetes; kidney failure; and obesity increase your risk for PAD.
Diagnosis
SEE A VASCULAR SURGEON
You will be asked questions about symptoms and medical history, including questions about family members. The vascular surgeon will also perform a physical exam.
TESTS MAY BE RECOMMENDED
● Ankle-brachial index (ABI). This is a common test used to diagnose PAD. It compares the blood pressure in your ankle with the blood pressure in your arm.
You may walk on a treadmill and have readings taken before and immediately after exercising to capture the severity of the narrowed arteries during walking.
● Ultrasound. Special ultrasound imaging techniques, such as Doppler ultrasound, can help your doctor evaluate blood flow through your blood vessels and identify blocked or narrowed arteries.
● Angiography. Using a dye (contrast material) injected into your blood vessels, this test allows your doctor to view blood flow through your arteries as it happens. Your doctor is able to trace the flow of the contrast material using imaging techniques, such as X-ray imaging or procedures called magnetic resonance angiography (MRA) or computerized tomography angiography (CTA).
Catheter angiography is a more invasive procedure that involves guiding a catheter through an artery in your groin to the affected area and injecting the dye that way. Although invasive, this type of angiography allows for simultaneous diagnosis and treatment. After finding the narrowed area of a blood vessel, your doctor can then widen it by inserting and expanding a tiny balloon or by administering medication that improves blood flow.
● Blood tests. A sample of your blood can be used to measure your cholesterol and triglycerides and to check for diabetes.
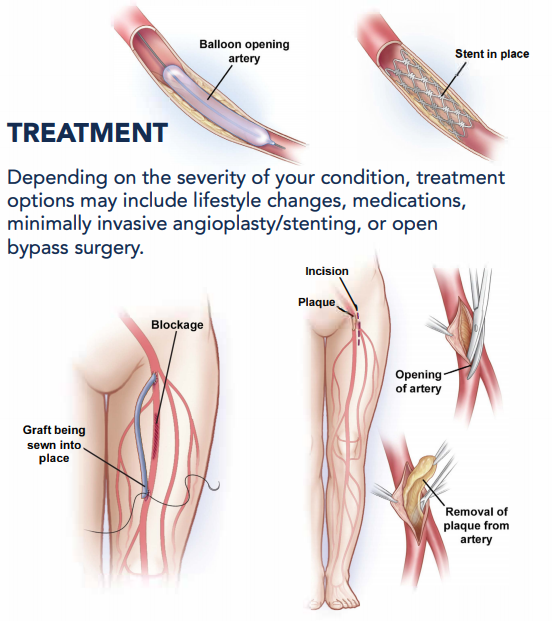
TREATMENT
PAD is usually treated by aggressively managing the risk factors with lifestyle changes and medication. This includes :
● Cholesterol-lowering medications. You may take a cholesterol-lowering drug called a Statin to reduce your risk of heart attack and stroke.
- High blood pressure medications: If you have high blood pressure, your doctor may prescribe medications to lower it.
- Controlling your blood sugar (glucose) levels becomes even more important while suffering from diabetes.
● Medications to prevent blood clots. PAD is related to the reduced blood flow to your limbs, it’s important to improve that flow. Your doctor may prescribe daily aspirin therapy or another medication, such as Clopidogrel (Plavix).
● Symptom-relief medications: The drug Cilostazol increases blood flow to the limbs both by keeping the blood thin and by widening the blood vessels. It specifically helps treat symptoms of claudication, such as leg pain, for people who have peripheral artery disease. Common side effects of this medication include headache and diarrhea. Not all patients benefit from this medicine
Angioplasty and surgery
In some cases, angioplasty or surgery may be necessary to treat peripheral artery disease that’s causing claudication:
● Angioplasty. In this procedure, a small hollow tube (catheter) is threaded through a blood vessel to the affected artery. There, a small balloon on the tip of the catheter is inflated to reopen the artery and flatten the blockage into the artery wall, while at the same time stretching the artery open to increase blood flow.
Your doctor may also insert a mesh framework called a stent in the artery to help keep it open. This is the same procedure doctors use to open heart arteries.
● Bypass surgery. Your doctor may create a graft bypass using a vessel from another part of your body or a blood vessel made of synthetic (man-made) fabric. This technique allows blood to flow around — or bypass — the blocked or narrowed artery.
● Thrombolytic therapy. If you have a blood clot blocking an artery, your doctor may inject a clot-dissolving drug into your artery at the point of the clot to break it up.
Symptoms
MAY HIDE
Many patients may not experience or may ignore their symptoms.
FATIGUE OR CRAMPING OF MUSCLES WHILE WALKING
Fatigue or cramping of your muscles (claudication) in the calf, thigh, hip, or buttock may signal you have PAD. Typically the discomfort is felt after walking a certain distance and goes away with rest.
PAIN IN TOES OR FEET WHILE RESTING
If you have pain in your toes or feet while resting, you may have an advancing case of PAD.
OPEN WOUND ON TOES OR FEET
An open wound or ulcer on your toes or feet, often at a pressure point on the foot, can signal a serious case of PAD. An ulcer can progress to gangrene. These symptoms require immediate medical attention.
SOME OTHER signs and symptoms may include:
● Leg numbness or weakness
● Coldness in your lower leg or foot, especially when compared with the other side
● A change in the color of your legs
● Hair loss or slower hair growth on your feet and legs
● Slower growth of your toenails
● Shiny skin on your legs
● No pulse or a weak pulse in your legs or feet
● Erectile dysfunction in men
Causes
● Smoking
● Diabetes
● Obesity (a body mass index over 30)
● High blood pressure
● High cholesterol
● Increasing age, especially after reaching 50 years of age
● A family history of peripheral artery disease, heart disease or stroke
● High levels of homocysteine, a protein component that helps build and maintain tissue
People who smoke or have diabetes have the greatest risk of developing peripheral artery disease due to reduced blood flow.
Staying Healthy
The best way to prevent claudication is to maintain a healthy lifestyle. That means:
● Quit smoking if you’re a smoker.
● If you have diabetes, keep your blood sugar in good control.
● Exercise regularly. Aim for 30 to 45 minutes several times a week after you’ve gotten your doctor’s OK.
● Lower your cholesterol and blood pressure levels, if applicable.
● Eat foods that are low in saturated fat.
● Maintain a healthy weight.
Take prescribed medications as recommended to control high blood pressure, high cholesterol or triglycerides, diabetes, and kidney failure.
Eat a balanced, low-sodium, low-fat diet.